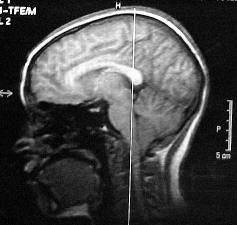
 The Hashimoto's Brain? Idiopathic Symptoms  Many people report cognitive and memory problems with hypothyroidism. The reason for these symptoms are often not identified nor really known. Hypothyroidism effects our bodies in many ways and apparently can aggravate other conditions. These other conditions may have been subclinical and never diagnosed because the symptoms were very minimal and posed no significant problems. When the metabolism of the body is adversely effected this can cause symptoms to become worse. I have recently learned what one of these "subclinical conditions" were, Attention Deficit Hyperactivity, Predominately Inattentive Type (ADHD). I am still learning about this but it does help me to know the reason for the "problems" and bothersome "squerks". I will describe these cognitive problems here and identify what the causes of the symptoms I know as well as the other symptoms I'm still searching. Processing Information: The brain thinks and processes information in slow motion. There is a significant decline in these cognitive abilities from what they were prior to getting hypothyroidism. The person can't read fast or speak quickly. It's like the brain does not "think clearly" and is stuck in slow gear. It's just in slow motion. The neurons are passing the messages through the synapses extremely slow. All creativity during this time seems to be lost. You can't think so you can't come up with new ideas. However a few hours later the brain seems to work better and can think faster and clearer. (This is possibly partly due to a learning disability I was born with, due to being a premie. Stress and hormonal factors exagerate the symptoms after developing the hypothyroidism.) Memory: The brain is unable to pull stored information from memory. Many people experience this from time to time but many people with hypothyroidism will feel they got dementia (maybe they do have "mild dementia" referred to in the latest medical news). They even have problems recalling names of common objects. This really interfers with social life because they can't remember what is happening in their friends' lives. This can be a problem at work because they can't remember what they did or didn't do at work. (No clue yet but still looking.) Easily Distracted: Another problem is a significant level of distractibility. They are unable to hold a trend of thought or carry on a conversation in a noisy environment. They have extreme problems carrying on a conversation when someone else is carrying on another conversation in the same room or if the TV is on. They sometimes get distracted by their own thoughts. They can definitely sympasize with people who have attention deficit problems. This can be the most frustrating aspect of the disease. (This is the main symptom of my ADHD.) Brief Blockage in Information Reception: Many people may also experience brief transient brain gaps or blockage in receiving or comprehending information (lasts for just a split second or so) which is only noticed during conversations or listening. It seems that a word or two is left out of the conversation. (Ex. George got ----- --- ----- when he was out yesterday.) The thyroid person would ask "What did he get?) There is no seizure activity that is revealed by medical tests. It's just as if the brain shuts down for a second or so, the person is still fully conscious and alert. It's just that the person misses out on what was just said. This is also a very frustrating thing and tends to lead to the hypothyroid person to be introverted and socially withdrawn to avoid this frustration. (Partly due to the ADHD. This may also be caused by the other learning disability and partly due to my ears not hearing.) DIFFICULTY STAYING AWAKE DURING THE DAY: As long as the person is busy and on the go there is no significant problem with sleepiness but as soon as the person stops and is still for a short period of time sleepiness comes in. During meetings, church services, movies or any activity where the person is sitting still for a period of 10-15 minutes there is an extreme sense of sleepiness which leads to doozing off. This sleepy spell may last anyway from 2-3 minutes to 5-10 minutes. It's as if when the brain gets enough stage 1 or sometimes stage 2 sleep it gets it's rest to carry on with it's normal activities. Also during these sleep attacks the brain may occasionally have auditory hallucinations such as hearing your name called or hearing a few words. The brain is starting to dream. (A subclinical case of narcolepsy? I joke about this but it seems the neurological system developed 98% instead of the 100% as is considered normal. Symptoms are insignificant but it does cause a few unseen problems.) DIFFICULTY CONCENTRATING: It's as if the brain forgets what this is. While reading it takes a paragraph or two to get in gear in understanding that the words are saying something. It can get bad enough that reading and comprehending what you read is out of the question. Anything that requires sustained attention is a real strain. It's like trying to run the extra mile when your body doesn't seem to have it in there to go. (Definitely the ADHD.) DIFFICULTY FOCUSING MY ATTENTION: It's a real effort. The brain feels like your muscles when you try to lift something that is almost too heavy to do. If you strain hard enough you can lift it for a few minutes but not for any extended period of time. The same thing with the brain. It can focus but only for about 30 seconds or so. Hearing a conversation all the way through doesn't happen. It is just extremely difficult to focus. Now things may attract the attention such as an action TV program or things of high level of interest. Generally we all have things we are more interested in. Needless to say what is easier to attract the attention can still get the attention but the attention span is much shorter than what it normally would be. (ADHD which is also aggravated by stress and fatigue. Stress and fatigue makes the symptoms worse than before the hypothyroidism.) DIFFICULTY KEEPING MY MIND FROM WANDERING: The brain is always thinking until it deteriates to the point there are no thoughts. I never really considered this that much of a problem because that's were great ideas come from. This web page is a good example of the brain wandering. As I got ideas I add them. As I experience something, learn something or am inspired by something I add it to the site. This can be a nuesense I guess for many people but I don't consider this any significant problem. It's only a problem during a depressive time because then all the thoughts are negative but again positive thoughts come in or I get tired of the negative thoughts and decide to "solve" the problem (ex. addressing the cognitive problems) (One of the potentially positive aspects of ADHD or what I consider a creative mind.) DIFFICULTY REMEMBERING INFORMATION: There are 3 types of memory. The Working Memory gathers all the experiences we have or things we see, hear, touch, taste, feel and sends them to the Short Term Memory. The Short Term Memory is where the phone numbers are held when someone tells you a number and you hold it in your head until you immediately dial the number. The Long Term memory is where information is stored. This is things we have learned, childhood or adult experiences, or what we call "memoriable memories". With hypothyroidism the working memory quits working. Therefore most things don't get into the memory. Needless to say it still works some but there is a significant decrease in the efficiency of the working memory causing things not to be remembered. (Partly due to the other learning disability but more since the hypothyroidism the memory problems has been worse. ADHD may be a contributing factor.) DIFFICULTY THINKING OF WORDS I WANT TO SAY: Everyone has this problem from time to time but with hypothyroidism (and other conditions which have similar cognitive problems) this occurs more often. It's an embarrishment at times which leads the person to feel less intelligent than others. It's not to the extent of alzheimer's but it is a noticable problem when combined with the other cognitive problems. (Not sure of the cause on this one.) DIFFICULTY THINKING CLEARLY: This is a frustrating condition because it just seems the brain isn't alert and sharp. It's slow and sluggish. It's like wearing dirty glasses. (May be partly due to a depression which I don't expect to be a significant problem anymore.) COLD EXPOSURE: Can adversly effect the cognitive abilities over extended period of time or have no effect or may wake up the brain and make it work a little clearer. EMOTIONAL STRESS: Definitely makes all cognitive and physical problems worse. Hormonal Fluxuations associated with PMS adversely effects cognitive functioning as well as mood & confidence. (ADHD does make a person more emotionally sensitive. Knowing the cause of the body's release of hormones causing stronger emotions helps me tramendously. Knowledge of the cause is very important to me. I can accept it if I know the reason.) PHYSICAL OVEREXERTION: Usually have no or little effect but sometimes can cause temporary decline in cognitive problems due to fatigue. Fibro Fog Follies These can also be called Human Brain Fog Follies. See how many you can relate to. Enjoy some laughs. We have to laugh at ourselves and look for similarities rather than differences. This helps us cope and be happier people. Remember the ABC's of Life. Cognitive Problems that may occur with thyroid and other autoimmune diseases Difficulty with simple calculations (e.g., balancing checkbook) Word-finding difficulty Saying the wrong word Difficulty expressing ideas in words Difficulty moving your mouth to speak Slowed speech Stuttering; stammering Impaired ability to concentrate (ADHD) Easily distracted during a task (ADHD) Difficulty paying attention (ADHD) Difficulty following a conversation when background noise is present (ADHD) Losing your train of thought in the middle of a sentence (ADHD) Difficulty putting tasks or things in proper sequence Losing track in the middle of a task (remembering what to do next) Difficulty with short-term memory Difficulty with long-term memory Forgetting how to do routine things Difficulty understanding what you read Switching left and right Transposition (reversal) of numbers, words and/or letters when you speak Transposition (reversal) of numbers, words and/or letters when you write Difficulty remembering names of objects Difficulty remembering names of people Difficulty recognizing faces (this is definitely a significant problem for me) Poor judgment Difficulty making decisions Difficulty integrating information (putting ideas together to form a complete picture or concept) Difficulty following simple written instructions Difficulty following complicated written instructions Difficulty following simple oral (spoken) instructions Difficulty following complicated oral (spoken) instructions (ADHD) Difficulty following directions while driving Becoming lost in familiar locations when driving Feeling too disoriented to drive  Hashimoto's Encephalopathy A Neuroendocrine Disorder Artical by Beverly Seminara, Patient Advocate "Hashimoto's Encephalopathy is a very rare and potentially deadly autoimmune disease with symptoms that can mimic many different neurological disorders. It is a treatable disorder -- if doctors figure out what it is in time and begin treating it. It is critical for the patient that doctors, neurologists and endocrinologists recognize this disease as soon as possible. When properly diagnosed and treated, patients begin positively responding within two weeks from the horrifying and most frightening symptoms. Hashimoto's Encephalopathy is a disease that may have a connection to Hashimoto's Thyroiditis. However, many patients were euthyroid (normal thyroid range) or hypothyroid upon onset. It must be made absolutely clear that just because someone is has Hashimoto's Thyroiditis or another thyroid problem, that does not mean that the individual is destined to develop Hashimoto's Encephalopathy - this condition is quite rare. Hashimoto's Thyroiditis was named after the Japanese physician Dr. Hakaru Hashimoto, who first described this condition in 1912. Hashimoto's Thyroiditis is the most common cause of hypothyroidism in the U.S., and is an autoimmune or chronic lymphocytic type of thyroiditis. Hashimoto's Thyroiditis is not uncommon. The thyroid gland typically becomes and the antibodies the body normally produces to protect the body and fight foreign substances such as bacteria, are found to 'attack' their own thyroid tissue. Thyroid antibodies are present in 95% of Hashimoto's Thyroiditis patients and the thyroid autoimmune antibody test serves as a marker for Hashimoto's Thyroiditis. Treatment is basically the treatment for hypothyroidisim - thyroid hormone replacement drugs. Hashimoto's Encephalopathy is quite a different situation. There are some conflicting views by researchers as to Hashimoto's Encephalopathy being a type of autoimmune cerebral vasculitis, a neuroimmunological syndrome, a neurological encephalopathy, a condition that develops due to Hashimoto's Thyroiditis, or perhaps a disorder that should be classified separately. What is known is that it is a neuroendocrine disorder - meaning it affects both the endocrine system, and the neurological (nervous) system. Hashimoto's Encephalopathy is underdiagnosed - it is likely that more cases exist than are actually properly diagnosed. It is also a treatable condition, but not curable, however, long term prognosis is good with proper treatment. It is also a relapsing condition, and a steroid responsive disorder, treatable with pral corticosteroids (Prednisone or its derivatives.) Hashimoto's Encephalopathy typically have high antithyroid antibody titers as do patients with Hashimoto's Thyroiditis, and all patients with Hashimoto's Encephalopathy eventually are diagnosed with Hashimoto's Thyroiditis as well. As with Hashimoto's Thyroiditis, antibodies attack the thyroid gland, but with Hashimoto's Encephalopathy, antibodies also attack neurons in the brain. The neurological symptoms frequently lead to mistaken neurological diagnoses. Many symptoms can occur. Some patients experience many of these symptoms, others may show some but not all of the symptoms listed here. Symptoms include: Confusion Disorientation Psychosis Coma Tremors Convulsions Concentration Problems Attention Span Problems Difficulty Retaining Information Short Term Memory Problems Seizure Activity Monoclonal Jerks - Involuntary Muscle Jerks Dementia Fatigue Coordination Difficulties Headaches Episodes of Stroke Episodes of Stroke-Like Deterioration Right Sided Hemiparesis - Right Sided Partial Paralysis Aphasia - Speech Difficulties Articulation Difficulties Word Finding Difficulties Fine Motor Movement Problems - Coordination of arms, hands, fingers. It's easy to see how, with these types of symptoms, a patient could easily be misdiagnosed with many other neurological disorders, such as stroke, early dementia, Alzheimers, psychosis, Wilson's Disease, Pick's Disease, brain cancer, primary progressive aphasia, and others. (Those are just a few of the misdiagnoses I personally had. Can you imagine being told you have one of these and to: "Get your affairs in order, you will be in a nursing home in six months or six years.") If Hashimoto's Encephalopathy is misdiagnosed, the lack of proper treatment can result in irreversible dementia, coma or even death. Remember it is treatable, and with proper treatment, long term prognosis is good. I know. It's a terrifying disease. I have had Hashimoto's Encephalopathy since the summer of 1995. I went untreated for three years. My condition continued to deteriorate. I went from neurologist to neurologist even with a case study in hand on Hashimoto's Encephalopathy, with the recommended treatment, and still I did not receive the treatment specified by the case study -- oral corticosteroids - commonly known as Prednisone. It wasn't until I finally found an endocrinologist who acknowledged its existence, even though he had never heard of it. He seriously considered the case study and welcomed the challenge of something new, something not in the textbooks. We worked as a team and began treatment with Medrol, a form of Prednisone. It took us one year, beginning in October 1998, starting off at extremely high doses and suffering all the horrible side effects that come with it, to find my "Magic Number" - the perfect number of milligrams that treats my condition. We found that number in the spring of 1998, only after I had to suffer a relapse to know for sure that 6 mgs. was too high, and 2 mgs. was too low, that 4 mgs. a day is what I needed. In the beginning of this disease and experiencing some or many of the symptoms mentioned, many patients undergo extensive neurological testing' as a course of process of elimination. Finally, if they are lucky, they receive the correct diagnosis. The endless neurological tests performed may often be normal, or may show an irregular EEG, or in some cases MRI testing show some atrophy within the brain. If an endocrinologist is called in, tests may show that the euthyroid patient is now hypothyroid and all patients now have Hashimoto's Thyroiditis. The Thyroid Autoimmune Antibody Test will show high titers of antithyroid antibodies. The good news for patients who are lucky enough to receive the correct diagnosis and proper treatment, is that long term prognosis is good with this often underdiagnosed disease. I can only speak from my own experience with Hashimoto's Encephalopathy, even with the knowledge that a relapse can happen at no given internal, or that it could be triggered by stress or just being overtired, or perhaps someday maybe I may be one of the few fortunate patients that actually goes into total remission, or maybe not. Having Hashimoto's Encephalopathy changes you, yes. Perhaps you are not exactly how you were before, but you're alive, functioning, able to perform daily routine activities, be independent. The relapse that may occur is correctable. I may have a relapse next week, maybe not for months, years. It is unpredictable. But when/if it does happen, correcting it for me, is just upping my milligrams from 4 mgs. a day to 6 mgs. for two or three days. No side effects from the medication and most important the relapse is gone and I am as I was before. Interestingly, 34 case studies on Hashimoto's Encephalopathy have been published since 1966, and still this disease is underdiagnosed and misdiagnosed. The majority of cases are women. But it is imperative to note that this disease knows no gender or age. Case studies show ages 12 to 82 afflicted and just recently, titles indicating Pediatric Hashimoto's Encephalopathy. Studies are from all over the world and include multiple patients in each study. India, Italy, Greece, Scotland, Norway, The Netherlands, Spain, Japan, Germany, Great Britain, France, etc. So far only 10 people have been published in case studies within the United States. But they haven't added me or one other young woman I know who was recently diagnosed. That makes 12 of us in the United States, plus how many more in the other countries? We were diagnosed and treated. The question is: How many more are there? Misdiagnosed? Suffering needlessly? Hospitalized, or institutionalized needlessly? In psychiatric institutions needlessly? In nursing homes needlessly? Dying needlessly? Makes you wonder. For many patients, the neurological symptoms will appear first. Specialists are often will be unable to make a clear diagnosis. Many may receive a neurological diagnosis often ending with - 'of unknown etiology,' meaning of unknown cause. I did. Too many are being misdiagnosed. If I had not challenged the doctors, educated myself on every medical term and test, asked question after question, been so determined and tenacious to pursue my "Final Diagnosis of Primary Progressive Aphasia of Unknown Etiology," I would not be here today. I am passionate about this underdiagnosed disease, desperately want to let people know, especially neurologists and endocrinologists, that when they have that one patient exhibiting such symptoms and medical testing is so inconclusive for any disease they already know : Think, could this be Hashimoto's Encephalopathy? Then they will again save another life."  This artical by Dr. Bruno farther explains the word finding difficulty which many people who don't have the medical conditions he mentions also experience.  August, 2002 by Dr. Richard L. Bruno Q Do CFS patients have progressive memory loss? When I am very fatigued or stressed I am unable to remember the word I was going to say. I'm frightened. Am I getting Alzheimer's disease along with CFS? A No, what you describe isn't Alzheimer's. You are experiencing word-finding difficulty which has nothing to do with memory loss or Alzheimer's disease. Like so many fatigue-related problems in people with CFS/ME, word-finding difficulty is also reported by polio survivors with "brain fatigue." In our 1990 International Survey 79% of polio survivors reported difficulty "thinking of words I want to say." Thirty-seven percent reported frequent, moderate-to-severe word-finding difficulty. Polio survivors and CFS patients have difficulty naming objects and sometimes even getting out the names of people they know well! But word-finding difficulty is not associated with memory loss or thinking problems, symptoms of Alzheimer's disease. It is related to trouble focusing attention and a decrease in bran activation, the fundamental problem we think underlies "brain fatigue." In one study we found that difficulty with word-finding and focusing attention were related to polio survivors' brains making less dopamine. Recent studies have found that CFS and fibromyalgia patients make less dopamine, too. (Neurons that make dopamine are killed by a number of encephalitis-causing viruses in addition to the polioviruses.) Why is too little Dopamine related to trouble "finding" words? Dopamine is not only the main brain activating neurochemical. Dopamine also connects the two "talking" parts of the brain: the part that thinks of the word you want to say and the part that "says" it. If you have too little dopamine you can think of a word but you can't get it out. Knowing the word you want to say but not being able to say it is called the "tip-of-the-tongue" experience and is a common Parkinson's disease symptom. And that makes sense. Low dopamine is the cause of Parkinson's disease. We found that word-finding difficulty was as severe in polio survivors as it was in Parkinson's patients, even though polio survivors do not experience the tremor and rigidity of Parkinson's disease. However, there have been some CFS patients who, at least immediately after they became ill, did have some Parkinson's-like tremor and rigidity. In 1996 we published a study showing that bromocriptine, a dopamine-replacing drug, reduced word-finding difficulty, attention problems and fatigue in polio survivors. However, medication is not necessary to treat word-finding difficulty. Reducing physical and emotional stress decreases fatigue, word-finding difficulty and all brain symptoms in polio survivors and CFS patients. If you're having trouble thinking of a word that you want to say, take a rest break, a deep breath and try to "talk around" the word by describing the thing you're trying to name. If you are forgetting your friends and relatives names, just call everyone "Buddy" or "Honey."  Dr. Richard Bruno is Director of Fatigue Management Programs and The Post-Polio Institute at Englewood (NJ) Hospital and Medical Center. His new book, THE POLIO PARADOX: UNCOVERING THE HIDDEN HISTORY OF POLIO TO UNDERSTAND TREAT "POST-POLIO SYNDROME" AND CHRONIC FATIGUE, is published by Warner Books. (AOL Keyword POLIO PARADOX.) E-mail questions to him at:PolioParadox@aol.com Archives of Co-Cure@listserv.nodak.edu  All of these things do lend to negative thoughts and frustrations. Is there anything that can be done to help this? However I must always remind myself to trust in the Lord, rely on Him to work through me to help others as well as learn what he wants me to learn through this. As Paul prayed for the "thorn in his flesh to be removed" the Lord gave him grace and helped him learn to trust in the Lord despite the "thorn in his flesh". There is a reason for everything. I have always been a worrying overly sensitive person. However I am learning to make positive changes in my attitude and now have to "resolve problems" rather than worry about them. Anyone who really knows me knows that I can't just live with a problem. I have to fix it, if that's possible. If there is nothing that can be done to fix it then I just have to forget it. I can afford to keep it in my mind because I am becoming physically "allergic" to my stress hormones. (High levels of my stress hormones causes physical aches, pains & fatigue that lasts about 1-2 days.) I know when ever I really get emotionally upset I will pay the consequences of it. It's too bad that everyone in the world isn't like this. Just think what would happen if everyone had this reaction. If they don't like physical pain and had the slightest bit of common sense, they would avoid the things that cause the high stress hormones. Therefore I have to focus more on the Lord and eternal things rather than things of this world. This will help me to keep everything in proper perspective.  Cognitive Problems Related Links  Neurology Channel: Fibromyalgia "Causes of fibromyalgia are not known. The condition produces vague symptoms that may be associated with diminished blood flow to certain parts of the brain and increased amounts of substance P, which is thought to be a sensory neurotransmitter involved in the communication of pain, touch, and temperature from the body to the brain. Researchers have identified several other possible causes, including the following: Autonomic nervous system dysfunction Chronic sleep disorders Emotional stress or trauma Immune or endocrine system dysfunction Upper spinal cord injury Viral or bacterial infection" Sustained Reduced Sleep Can Have Serious Consequences"According to Principal Investigator David Dinges, "This is the first systematic study to look at the prolonged cognitive effects of chronic sleep restriction lasting for more than a week. The results provide a clearer picture of possible dangers to people who typically are awake longer on a regular basis," he explained, "including members of the military, medical and surgical residents, and shift workers. Reduced cognitive abilities can occur even with a moderate reduction in sleep." Cognitive performance deficits included reduced ability to pay attention and react to a stimulus, such as when driving, or monitoring at airports. Other deficits involved impairment of the ability to think quickly and not make mistakes, and a reduced ability to multi-task -- to hold thoughts in the brain in some order while doing something else. Investigators also found that to prevent neurobehavioral defects from accumulating, the average person needs 8.16 hours of sleep during a 24-hour day, although there were differences among individuals in their need for sleep." When depression can be caused by hypothyroidism Depression can be caused by an imbalance of the thyroid hormones. Depression is a terrible feeling however there need not be a void in your life. There is a certain size space in everyone's heart which God has created that thirsts for Him. He gives us a sense of peace and knowledge that He will work all things out and I know I have to trust Him. He also teaches me to learn from each experience and to see what good can come from it. This site gives farther explaination of God's relationship with people. Depressed patients respond well to Vitamin B Supplements "New research reports, patients who were treated for depression responded better if they had a higher level of vitamin B12 in their blood. ...Researchers report the patients who responded fully to treatment had higher concentrations of vitamin B12 in their blood at the start and end of the study when compared to those who did not respond to treatment. The study also found the association between vitamin B12 and the response to treatment remained even after other factors were considered such as type of treatment received, smoking and drinking habits, and if other family members suffered from depression." Stress related symptoms I have experienced and how I coped with them. But those who wait for the LORD shall renew their strength, they shall mount up with wings like eagles, they shall run and not be weary, they shall walk and not faint. Are you feeling stress? Information on coping with stress from symptoms and life in general. I hope you find this helpful. Stinking thinking & fatigue This is an email I got which I really want to share. The ideas shared are truely effective in reducing stress and stress related symptoms which people with autoimmune diseases are apparently more prone to experience and stress does aggravate health conditions as well. Predictors of low back pain onset in a prospective British study. An example of the adverse effects of stress. "RESULTS: Incident pain was elevated among those with psychological distress at 23 years of age (adjusted odds ratio [OR] = 2.52, 95% confidence interval [CI] = 1.65, 3.86) and among persistent moderate or heavy smokers (adjusted OR = 1.63, 95% CI = 1.23, 2.17). Significant univariate associations involving other factors (e.g., social class, childhood emotional status, body mass index, job satisfaction) did not persist in multivariate analyses. CONCLUSIONS: This prospectively studied cohort provides evidence that psychological distress more than doubles later risk of low back pain, with smoking having a modest independent effect. Other prospective studies are needed to confirm these findings before implications for low back pain prevention can be assessed." What's causing your headaches? "RealAge Headache Center For personalized advice on headaches and migraines, choose one of the four free health assessments today." Living with Memory Problems Hashimoto's & other autoimmune diseases can adversely effect underlying problems such as learning disabilities (LD). This is apparently what happened in my case. This was good because I'm learning a little LD can cause a lot more problems, besides bad spelling, which can cause depression. Jennifer's Thyroid Story A visitor to my site emailed me. She shared she also has problems with poor memory & a mild case of ADD. She has written 7 cookbooks. 5 Splendid Low-Carb Splenda® Cookbooks If you seriously struggle with your weight you may want to check out her cookbooks. Thyroid Support This page includes links to active egroups (online electronic support groups) for support and informative newsletters on thyroid disease. I also share some ideas for coping with cognitive defects not corrected by T3 & T4 replacement and dietary supplements hasn't helped. The Potter's Hand Prayer & Support Group meets the 2nd & 4th Tuesdays of each month 7:00pm-8:30pm in Crosstracks, (located in the lower level of the Family Life Center building) at Central Church of God corner of Sardis & Randolph Rds 5301 Sardis Rd Charlotte. The group prays, discusses how to glorify God in difficult circumstances, and provides a networking opportunity to share useful information. The group is open to people with disabilities, family members, caregivers, teachers, and people with a heart to help. Everyone is welcome. Hold Your Head High! A short inspirational poem which offers words of encouragement. "Stopping at nothing and doing what's in your heart that you know is right ...is Determination." Herbs & Vitamins I have found to be helpful for people living with stress. I have been taking an herb for a few years now and so far I have found it has greatly improved and restored about 50% (or more) of my cognitive abilities. Myra Preston PhD Clinical psychophysiologist/neurophysiologist Siber Imaging (brain mapping) Charolotte NC Siber Imaging (brain mapping) It's an expensive program but has helped people retrain their brains to improve the neurons firing messages & brain waves.  A Prayer Father, I ask you to bless my friends reading this right now. I am asking You to minister to their spirit at this very moment. Where there is pain, give them Your peace and mercy. Where there is self doubting, release a renewed confidence in Your ability to work through them. Where there is tiredness, or exhaustion, I ask You to give them understanding, patience, and strength as they learn submission to your leading. Where there is spiritual stagnation, I ask You to renew them by revealing Your nearness, and by drawing them into greater intimacy with You. Where there is fear, reveal Your love, and release to them Your courage. Where there is a sin blocking them, reveal it, and break its hold over my friend's life. Bless their families, meet their needs, give them greater vision, and raise up leaders and friends to support and encourage them. Give each of them discernment to recognize the evil forces around them, and reveal to them the power they have in You to defeat it. I ask You to do these things in Jesus' name.  Other Links  Neuropsychological functioning in chronic fatigue syndrome: a review These memory problems can also accompany many people who have Hashimoto's. Education, Equity and Cognitive Dysfunction Dilemmas "This paper addresses the issue of the Cognitive Dysfunction of ME/CFS affecting education and educational outcomes for students and also how the present system leaves vulnerable medical practitioners, disability officers, academics and teachers under the Federal Disability Discrimination Act, 1992." What is Brainfog and How Significant Is It? Artical descibes cognitive problems with fibromyalgia but these problems also occur with Hashimoto's & many other autoimmune conditions. Cognitive Function & Fibromyalgia "However, we have found that FM patients perform more poorly than age- and education-matched controls on tests of several different types of cognitive function. For example, FM patients could recall fewer words when given a list of words to remember and recall later. FM patients also performed more poorly on a test of working memory. Working memory refers to your ability to hold something in mind briefly while you use that information for some other mental process. It is your mental desktop. Multiplying large numbers in your head is a good example of a task that uses working memory. In addition, FM patients had lower scores on vocabulary tests, and had lower scores on a verbal fluency test. In the verbal fluency task, people are shown a letter and are asked to write down as many words as they can think of that start with that letter. It tests how quickly you can access your stored knowledge of words. Thus, our results show that FM patients do indeed have some cognitive dysfunction. In fact, the cognitive performance of FM patients was equivalent to that of adults who were twenty years older than the FM patients on several of our tests. Moreover, the FM performance and that of the older adults was worse when compared to control subjects the same age, gender, and education level as the FM patients. Our research on aging shows that memory declines reliably every decade, and our results with FM patients suggest that FM patients were cognitively twenty years older in their performance on some tasks. However, there was one key difference between the FM patients and the older controls. Older adults are typically slower than young adults on cognitive tests that measure how rapidly they process information. This slow processing explains many other symptoms of cognitive aging. But the FM patients were faster than the older adults, and in fact, were just as fast as the younger, age-matched controls. So although FM patients may perform similarly to older adults on some cognitive tasks, the underlying cause is not likely the same. In conclusion, our research has shown that patients' complaints about their cognitive problems are accurate: there is cognitive dysfunction in FM patients and this is not due solely to psychiatric disorders such as depression, or to other symptoms of FM such as sleep disturbance, anxiety or fatigue. On the other hand, cognitive dysfunction in FM is related to pain. Our future research will focus on the relationship of pain and cognitive function, as well as on some other types of cognitive tasks. Since many patients complain of difficulty focussing on one task, we plan to study attention in FM. Finally, we are planning some neuroimaging studies where we can see which parts of the brain are active during a cognitive task. We hope to find differences between the FM patients and healthy controls that will give us more information about this disorder." I wouldn't be surprised if they find that the cognitive problems are actually due to neurological changes and abnormalities and the pain of FM effects the brain in the same manner as other types of chronic pain conditions which do not actually have these cognitive problems. There are too many people who have the same cognitive problems described who do not have any chronic pain that effects their lives like FM pain sufferers do. Retinopathy Associated With Cognitive Impairment in Middle Age "NEW YORK (Reuters Health) Jun 06 - The results of a study published in the June issue of Stroke suggest that there is an independent association between retinopathy and cognitive impairment in middle-aged individuals who have not had a stroke. Dr. Tien Yin Wong, of the National University of Singapore, and colleagues examined the association between retinal microvascular abnormalities and cognitive impairment in 8734 middle-age subjects every 3 years from 1987 to 1998. At baseline, all of the subjects, who were participants in the Atherosclerosis Risk in Communities study, had not experienced a stroke. During patient office visits, the researchers obtained retinal photographs and examined them for retinal microvascular abnormalities. Standardized tests, including the Delayed Word Recall Test, Digit Symbol Subtest, and Word Fluency Test were then used to assess cognitive function. Retinopathy was associated with lower cognitive test scores after adjustment for education, diabetes, blood pressure, carotid intima-media thickness and other risk factors. "The adjusted odds ratios for persons with Delayed Word Recall scores 2 SD or lower than the mean were 2.60 for any retinopathy, 3.00 for microaneurysms, 3.39 for retinal hemorrhage, and 3.07 for soft exudates," the team reports. Because diabetes and hypertension are known to influence retinopathy and cognitive function, the team repeated the analyses in subjects with and without these conditions. The results of the cognitive tests were similar in both groups. These results suggest that cerebral microvascular disease may play an important role in the pathogenesis of cognitive impairment, Dr. Wong and colleagues note. "Longitudinal data may clarify the temporal sequence of these associations and the eventual clinical significance of these small, early cognitive function changes."" Prevalence of Neuropsychiatric Symptoms in Dementia and Mild Cognitive Impairment "Context Mild cognitive impairment (MCI) may be a precursor to dementia, at least in some cases. Dementia and MCI are associated with neuropsychiatric symptoms in clinical samples. Only 2 population-based studies exist of the prevalence of these symptoms in dementia, and none exist for MCI. Objective To estimate the prevalence of neuropsychiatric symptoms in dementia and MCI in a population-based study. Design Cross-sectional study derived from the Cardiovascular Health Study, a longitudinal cohort study. Setting and Participants A total of 3608 participants were cognitively evaluated using data collected longitudinally over 10 years and additional data collected in 1999-2000 in 4 US counties. Dementia and MCI were classified using clinical criteria and adjudicated by committee review by expert neurologists and psychiatrists. A total of 824 individuals completed the Neuropsychiatric Inventory (NPI); 362 were classified as having dementia, 320 as having MCI; and 142 did not meet criteria for MCI or dementia. Main Outcome Measure Prevalence of neuropsychiatric symptoms, based on ratings on the NPI in the previous month and from the onset of cognitive symptoms. Results Of the 682 individuals with dementia or MCI, 43% of MCI participants (n = 138) exhibited neuropsychiatric symptoms in the previous month (29% rated as clinically significant) with depression (20%), apathy (15%), and irritability (15%) being most common. Among the dementia participants, 75% (n = 270) had exhibited a neuropsychiatric symptom in the past month (62% were clinically significant); 55% (n = 199) reported 2 or more and 44% (n = 159) 3 or more disturbances in the past month. In participants with dementia, the most frequent disturbances were apathy (36%), depression (32%), and agitation/aggression (30%). Eighty percent of dementia participants (n = 233) and 50% of MCI participants (n = 139) exhibited at least 1 NPI symptom from the onset of cognitive symptoms. There were no differences in prevalence of neuropsychiatric symptoms between participants with Alzheimer-type dementia and those with other dementias, with the exception of aberrant motor behavior, which was more frequent in Alzheimer-type dementia (5.4% vs 1%; P = .02). Conclusions Neuropsychiatric symptoms occur in the majority of persons with dementia over the course of the disease. These are the first population-based estimates for neuropsychiatric symptoms in MCI, indicating a high prevalence associated with this condition as well. These symptoms have serious adverse consequences and should be inquired about and treated as necessary. Study of neuropsychiatric symptoms in the context of dementia may improve our understanding of brain-behavior relationships." Aggressive Lipoprotein Level Management May Prevent Cognitive Decline "Maintaining healthy levels of total and LDL cholesterol may inhibit cognitive decline in elderly women, California investigators report in the Archives of Neurology for March." Lowly Cytokine May Play Role In Controlling Neurotransmitters COLUMBUS, Ohio -- Researchers here in collaboration with a group in California have discovered that a protein normally thought only to be a component in the immune system actually plays a key role in regulating neurotransmission in the central nervous system -- the CNS -- as well. The protein, tumor necrosis factor alpha, or TNF-alpha, has long been known to be a key player in controlling cell death but this new finding offers new insights into how cells interact within the human nervous system. Understanding this new role of TNF-alpha may provide researchers with possible new approaches to treating illnesses such as dementia, Alzheimer's disease, stroke, epilepsy and spinal cord injury. The report was published in the latest issue of the journal Science. The findings by Jacqueline Bresnahan, professor of neurosciences at Ohio State University; Michael Beattie, professor and chair of the same department, and colleagues at Stanford University, show that TNF-alpha is vital for controlling the strength of signal transmission between nerve cells. And the level of signal strength may play an important role in determining how nerve cells respond to injury. Researchers have long believed that neurons were the most important cells in the nervous system because they controlled the passage of signals throughout the CNS. They thought that glial cells -- astrocytes, oligodendrocytes and microglia -- only performed a support role for those neurons, providing oxygen and nutrients to the neurons, shielding neurons from each other, and basically cleaning up dead neurons. The new research, however, points to a much greater role for the glial cells since they can manufacture and release TNF-alpha into the CNS environment. The TNF-alpha apparently is able to regulate the expression of certain neurotransmitter receptors on the surface of neurons. The more of these receptors there are on the surface of the neuron, the more signals it can transmit. In this case, the signals arise from the binding of glutamate molecules from the fluid surrounding the cell to these receptors. When the glutamate and receptor meet, a nerve impulse, or signal, is produced. The more receptors present, the more signals are increased. Normally, the cytokine TNF-alpha is released as part of the inflammatory process following an injury to the cells. Based on discussions with other Ohio State colleagues on how the brainstem sends "nausea signals" to the stomach, Beattie and Bresnahan remembered that when TNF-alpha and glutamate are both present, cell signaling activity seemed to increase. "We wondered that since there was glutamate and TNF-alpha present in the spinal cord after injury, then maybe TNF-alpha is actually enhancing the killing effect of the normal neurotransmitter," Beattie said. In testing this, they exposed nerve cells first to glutamate and then to TNF-alpha. Separately, neither had an impact on the normal killing effect. But when they exposed the cells to even small amounts of both compounds, the killing effect increased 120 percent. "This was a complete surprise and validated our hypothesis," Bresnahan said. The real question, however, was in the details of the process -- how exactly was the killing effect enhanced. For help with the answer, they turned to Beattie's brother Eric, a post-doctoral researcher at Stanford. The lab in which Eric Beattie was conducting research was looking at the role glutamate played in signal transmission in learning and memory. "We wanted to know if TNF-alpha was regulating the number of receptors on the cell surface," Bresnahan explained. "If the number of receptors increased, and if there was glutamate nearby to bind to them, that would allow more calcium into the cells, killing them." Experiments at the Stanford lab were able to show that controlling the presence or activity of TNF-alpha had a direct relationship to the numbers of glutamate receptors on the cell surface and therefore on the amount of synaptic transmission. "This showed that TNF-alpha, this cytokine that is supposed to come from the immune system and not have a role in transmitting information, is actually a potent modulator of neurotransmitter interaction," Beattie said. Beattie and Bresnahan's work has now turned to how this process affects the speed at which nerve cells die, adding that a host of illnesses are caused by a degeneration of neurons. Their work was supported by grants from the National Institutes of Health. Article: Ohio State University 23-Mar-02 Cognitive & perceptual Problems in MS This is a site on Multiple Sclerosis but the description of the cognitive problems are also common with Hashimoto's Thyroiditis & Hypothyroidism. Mild Cognitive Impairment Overview "Normal memory changes associated with aging are characterized by momentary lapses, such as misplacing an item, forgetting someone's name, or forgetting to pick up something at the store. In contrast, memory loss associated with MCI is a more persistent and troublesome problem. People with MCI have much greater difficulty, for example, remembering a fact after a relatively short time. In cognitive testing, people with MCI, after a delay, remember significantly less of a paragraph they have read or details of simple drawings they have seen compared to people with normal memory changes associated with aging. A person with MCI is likely to forget important events repeatedly, while significant information is retained in normal aging." US to Pay for Brain Scans to Diagnose Alzheimer's "September 16, 2004 Elderly patients who show signs of Alzheimer's will be able to get brain scans under the government's Medicare program, U.S. officials said on Thursday, a step which could lead to earlier diagnosis and treatment. Medicare will cover the positron emission tomography, or PET, scans for those patients who show signs of both Alzheimer's and dementia but whose final diagnosis "remains uncertain," as well as other patients who enroll in certain clinical trials, officials said. The Centers for Medicare and Medicaid Services last year decided against covering the scans for Alzheimer's, saying reimbursement would not lead to more accurate diagnoses or better treatments. On Thursday, the agency said it made its final decision in support of the payments on Wednesday after months of meeting with experts, advocacy groups and others." Diet Rich in Omega-3 Fatty Acid DHA Protects Brain Against Alzheimer’s Disease, UCLA Study Shows "UCLA neuroscientists have shown for the first time that a diet high in the omega-3 fatty acid DHA helps protect the brain against the memory loss and cell damage caused by Alzheimer's disease. The new research suggests that a DHA-rich diet may lower one's risk of Alzheimer's disease and help slow progression of the disorder in its later stages. The journal Neuron reported the findings on Sept. 2. "This is the first proof that our diets affect how our brain cells communicate with each other under the duress of Alzheimer's disease," said Greg Cole, senior author and a professor of neurology at the David Geffen School of Medicine at UCLA. "We saw that a diet rich in DHA, or docosahexaenoic acid, dramatically reduces the impact of the Alzheimer's gene. "Consuming more DHA is something the average person can easily control," added Cole, associate director of the UCLA Alzheimer's Disease Research Center. "Anyone can buy DHA in its purified form, fish-oil capsules, high-fat fish or DHA-supplemented eggs."" Antidepressants promote brain cell growth in rats Dec 15, 2000 (Reuters) I found this interesting. "In a study conducted in rats, regular use of antidepressants promoted the growth of new cells in the hippocampus, an area of the brain where cells are known to waste away in people who are depressed. The hippocampus plays a role in learning, memory and mood. ... Previous research has shown that depression and stress--physical and psychological--can destroy neurons and prevent new cells from growing in the hippocampus. ...In rats treated with an antidepressant for 2 to 4 weeks, the number of brain cells in the hippocampus increased 20% to 40%, the authors report in the December 15th issue of The Journal of Neuroscience." American Academy of Neurology Site links to latest medical findings pertaining to dementia and mild cognitive impairment. American Neurological Association Neurosciences on the Internet A large site you can research information. Headaches Due to Myofascial Trigger Points Explaination of various types of headache pain including pain in the eyeballs. The Adult Chiari I Malformation It's a diviation from what is considered normal which may possibly contribute to some idiopathic symptoms especially problems with balance or headaches or neck pain. NINDS Chiari Malformation Information Page "What is Chiari Malformation? Chiari malformation (also called Arnold-Chiari malformation) is a condition in which the cerebellum portion of the brain protrudes down into the spinal canal. Chiari malformation may be congenital, associated with other anomalies including myelomeningocele, syringomyelia, and spina bifida. Hydrocephalus (increased intracranial pressure) may also occur. Symptoms most often begin during infancy, although they may be delayed until adolescence or adulthood. Symptoms usually include vomiting, muscle weakness in the head and face, difficulty swallowing, and varying degrees of mental impairment. Paralysis of the arms and legs may also occur. As they grow older, adults and adolescents with Chiari malformation who previously were asymptomatic may show signs of progressive brain impairment, such as involuntary, rapid, downward eye movements. Other symptoms may include dizziness, headache, double vision, deafness, an impaired ability to coordinate movement, and episodes of acute pain in and around the eyes." Brainstem conundrum: the Chiari I malformation. J Am Acad Nurse Pract 2001 Apr;13(4):154-9 Author: Mueller D. Affiliation: Division of Neurosurgery, University of Missouri Hospital and Clinics, USA. mailto:muellerdm@health.missouri.edu NLM Citation: PMID: 11930527 PURPOSE: To describe the Chairi I Malformation in relation to the anatomy of the brain and spinal cord, the common manifestations of the condition, diagnostic considerations, and management for the primary care provider. DATA SOURCES: Extensive review of the world-wide scientific literature on the condition, supplemented with actual case studies. CONCLUSIONS: The adult Chairi I Malformation is an insidious congenital brainstem anomaly that consists of caudal displacement of the cerebellar tonsils, brainstem and fourth ventricle into the upper cervical space, resulting in overcrowding of the posterior fossa. IMPLICATIONS FOR PRACTICE: Due to the vague, and often ambiguous presenting symptoms of Chiari I Malformation, many patients are misdiagnosed with conditions such as multiple sclerosis, fibromyalgia, chronic fatigue syndrome, or psychiatric disorders. Patients frequently experience symptoms months to years prior to accurate diagnosis and often incur irreversible neurologic deficits. Co-Cure Web Site: Has many great research articals on fibromyalgia, chronic fatigue and related conditions, including this artical on chiari malformation. Below is another short abstract I got from fibroml@topica.com Abstract - Otologic manifestations of Chiari I malformation Sperling, N. M., R. A. Franco, Jr., et al. (2001). Otology & Neurotology 22(5): 678-81. OBJECTIVE: To assess the prevalence of otologic symptoms in patients undergoing surgical decompression for symptomatic Chiari I malformation. STUDY DESIGN: Cross-sectional, prospective, nonrandomized. SETTING: Urban tertiary referral center. PATIENTS: Patients with Chiari I malformation before surgical intervention. INTERVENTIONS: None. MAIN OUTCOME MEASURE: Results of completed questionnaire. RESULTS: Sixteen consecutive patients with Chiari I malformation completed the self-administered questionnaire. Eighty-one percent of patients reported episodic aural fullness, 81% reported tinnitus, 69% reported vertigo, and 56% reported fluctuating hearing loss. Headaches were reported as frequently as aural fullness and tinnitus. CONCLUSIONS: Most patients with Chiari I malformation have symptoms that mimic primary otologic pathologic changes. The existence of common pathophysiologic mechanisms is proposed. Arnold-Chiari Malformation (ACM or CMI) and Syringomyelia (SM) information webpage Lots of links to various types of sites & articals on chairi malformation. World Arnold Chiari Malformation Association "Staffed by volunteers, the World Arnold Chiari Malformation Association is committed to providing support, current information, and understanding to those affected by the Arnold Chiari malformation and syringomyelia." Website for symptomatic short mm'ers -those under the traditional 5 mm Chiari threshold Site has lots of links to articals on "atypical" Chiari Malformations. American Syringomyelia Alliance Project Inc Includes a lot of info including symptoms of Chiari. What are the Symptoms? Many people with the Chiari I Malformation experience no symptoms. When symptoms are present, they usually do not appear until adolescence or early adulthood, but can occasionally be seen in young children. The majority of patients complain of severe head and neck pain. Headaches are often accentuated by coughing, sneezing or straining. Patients may complain of dizziness, vertigo, disequilibrium, muscle weakness or balance problems. Often fine motor skills and hand coordination will be affected. Vision problems can also occur. Some patients experience blurred or double vision, difficulty in tracking objects or a hypersensitivity to bright lights. Physical examination may reveal nystagmus (involuntary eye movements). Other symptoms include tinnitus (buzzing or ringing in the ear), hearing loss or vocal cord paralysis. Patients may have difficulty swallowing, frequent gagging and choking and, in some cases, sleep apnea may be present." Internet Mental Health Dementia diagnostic criteria and other general information. TREATMENT OF THE COGNITIVE SYMPTOMS OF DEMENTIA artical by John C. Morris, Washington University School of Medicine, St. Louis, MO. WHAT IS PRIMARY PROGRESSIVE APHASIA? This occurs more often in men. Primary Progressive Aphasia (PPA) is a disorder caused by degenerative diseases of the brain, in which speech and language functions deteriorate gradually over a period of years, while memory and other abilities remain relatively preserved.  Dementia Web Research and news on dementia. Catching Alzheimer's in Time Pencil-and-Paper Test May Predict Alzheimer's. "Researchers at the University of California at San Diego compared the results of cognitive skills tests completed by a group of 40 older adults, half of which were later diagnosed with Alzheimer's. They found a big difference between the two groups in the tests that required people to name common items from pictures and use 3-D blocks to copy printed block designs (a test that measures a skill known as visuoconstruction). Both of these tests detect problems with asymmetries or irregularities in the brain. The pre-Alzheimer's group had a significantly larger gap between their naming and visuoconstruction skills. And they had these gaps more often than the others. Researchers say that while the start of Alzheimer's is generally marked by an overall decline in brain function, those people in the pre-Alzheimer's stages may show subtle changes in one area of cognitive function before the global decline occurs. Compared to genetic testing that indicates a higher probability of developing the disease, the study authors say psychological testing can help indicate when it's time to start medication. Another study in the same journal suggests people who have a certain genetic variation that puts them at increased risk of developing Alzheimer's may have problems with spatial attention and working memory that are similar to those found in patients with the disease. Researchers say these people with the high-risk variation of the ApoE gene may lack a chemical in the brain that manages spatial attention and have difficulty shifting attention to different locations in a visual field or line of sight." The Seven Warning Signs of Alzheimer's Disease "The seven warning signs of Alzheimer's disease are: 1. Asking the same question over and over again. 2. Repeating the same story, word for word, again and again. 3. Forgetting how to cook, or how to make repairs, or how to play cards — activities that were previously done with ease and regularity. 4. Losing one's ability to pay bills or balance one's checkbook. 5. Getting lost in familiar surroundings, or misplacing household objects. 6. Neglecting to bathe, or wearing the same clothes over and over again, while insisting that they have taken a bath or that their clothes are still clean. 7. Relying on someone else, such as a spouse, to make decisions or answer questions they previously would have handled themselves." Understanding Stages and Symptoms of Alzheimer's Disease "Alzheimer's disease develops slowly and causes changes in the brain long before there are obvious changes in a person's memory, thinking, use of words or behavior." Subjective Complaints, Verbal Fluency, and Working Memory in Mild Multiple Sclerosis "In this study, it was demonstrated that even in the mild stages of the disease, MS patients complained of more subjective complaints than the controls. They also had a smaller speaking span than controls and a lower score on verbal fluency. The poorer performance of patients cannot be explained by variation in verbal intelligence, basic attention, speed of information processing, or executive skills as assessed by the WCST-m. The poor performance of the MS group cannot be attributed to MS-related sensorimotor deficits, as verbal tests were administered, and patients were not affected by visual or articulatory changes. Although 3 patients were recovering from an exacerbation at the time of testing and 9 patients had progressive disease, they did not perform as outliers on any of the measures, and repetition of the MANCOVA with these cases excluded did not reduce the significance of the group difference, F(1, 62) = 3.11, p = .001, when the cases with progressive MS were removed and F(1, 66) = 3.16, p = .001, when those in exacerbation were removed from the sample. The positive relationship between working memory and verbal fluency demonstrated here is in agreement with the previous findings of Daneman (1991) in a normal sample. Post hoc analysis of our data revealed that the problem lies not just with producing fewer words per minute. Rather, patients made about twice as many errors of production, for example, failure to complete a sentence and false starts. This indicates that MS patients may be making more errors than normal at a planning level of discourse production (Garrett, 1982; Holmes, 1988) as a result of reduced working memory capacity (Daneman, 1991; Howell, Saling, Bradley, & Berkovic, 1994; Just & Carpenter, 1992). Other possible reasons for poor performance are unlikely to account for the results given the normal performance of MS patients on tests of verbal-conceptual processing and short-term storage. In addition, patients did not produce more perseverative errors than controls on the WCST-m. In short, these results support the idea that capacity limitations in working memory underlie the verbal fluency problems experienced by MS patients. As hypothesized, working memory was related to generalized complaints, supporting the notion that working memory dysfunction underlies the subjective cognitive difficulties commonly reported by individuals in the clinical setting. It is interesting to note, however, that the mechanism underlying the complaints of mild MS patients appears to differ from that of the controls. The major determinant of general cognitive inefficiencies in the control group was variation in affective state. For MS patients, on the other hand, affective factors did not account for the findings, raising the question of organic causes, presumably cerebral MS pathology. This is in contrast to a recent study (Arnett, Higginson, Voss, Bender, et al., 1999) that found that of the three groups tested, namely, depressed MS patients, nondepressed MS patients, and normal controls, only the depressed patients were impaired on a test of working memory. The working memory test employed was different from that of this research, making it difficult to compare the studies. In any case, findings from this investigation are not clear-cut. The study failed, for example, to include neuroimaging data and a depressed control group. Thus, it was not possible to attribute the poor performance of the depressed MS group to psychological factors alone. Consistent with our findings, Arnett and coworkers stated, "Clearly, there are MS patients without current depression who experience significant deficits on working memory" (p. 554). Our findings help elucidate the nature of the cognitive difficulties experienced by people with mild MS. Knowledge about the role of working memory in everyday problems can benefit patient education and assist the formulation of practical strategies to facilitate performance of work and home duties. Patients might benefit from discussion of ways to control environ-mental demands on working memory capacity during speaking and other tasks involving working memory. This study also suggests that standard neuropsychological assessment, represented here by the Verbal Scale of the WAIS-R, and the Attention/ Concentration Index of the WMS-R, may be relatively insensitive to the subtle cognitive impairment experienced by patients with mild MS. It remains to be seen whether the Wechsler Adult Intelligence Scale-III (Wechsler, 1997), with its Working Memory Index, improves the sensitivity of assessment in this patient group." Unforgettable memory boosters Artical gives insight on how to promote improved health & functioning of the brain. "Recent research shows that adult brains do, in fact, generate new cells, repair atrophied or damaged nerve branches that receive and process information, and create new patterns and connections. To make sure that happens, Lawrence C. Katz, Ph.D. has created "neurobics" to stretch and challenge our brains. A professor of neurobiology at Duke University Medical Center, Dr. Katz's approach stimulates the brain to produce its own nutrients and expand its network of associations and connections. His program of exercises presents the brain with "nonroutine or unexpected experiences using various combinations of your physical senses--vision, smell, touch, taste, and hearing--as well as your emotional sense," he says in Keep Your Brain Alive (Workman Publishing Company, 1999). While simple and built into regular daily activities, neurobic exercises are not routine. Rather, novelty, diversity and multisensory associations are employed to give the brain a workout. Neurobic workouts can include showering with your eyes closed, brushing your teeth with your nondominant hand, having a sandwich for breakfast, or dessert before dinner. Move your body Cardiovascular health and the brain's neurotransmitters function better with regular exercise, and one study suggests exercise may increase IQ, notes Walter M. Bortz, M.D., Professor of Medicine at Stanford University School of Medicine and author of Living Longer for Dummies (Hungry Minds, 2001). "Nerve reaction time, which goes down with age, is improved with an exercise program," says this physician who practices what he preaches. At age 72, he told Well Journal, he will run the Boston Marathon this month. The brain is a muscle that needs physical stimulation and nurturing to grow and stay strong, Dr. Bortz says. "With exercise, you generate adrenaline, one of the prime neurotransmitters. It's the spark that gets the message from one nerve to the other." "  Other conditions effecting the functioning of the brain  Attention Deficit Disorder, Learning Disabilities & Neuroscience Attention Deficit Disorder NOS (not otherwise specified)is an apparent cause of many of the "cognitive problems" I shared on this site. Apparently the hashimoto's or hypothyroidism aggravated it, causing a worsening of the symptoms. However for the most part the symptoms have improved yet some areas remain and some of the ADD symptoms have always been an annoying problem especially socially. Information processing in chronic fatigue syndrome Research of comparison of cognitive abilities between people with CFS & healthy people. AAADD A little humor is good for the soul. Laughter is like medicine to the heart. We all need to use some humor with our goofy brains. Curry Spice May Slow Multiple Sclerosis Progression Our seasonings and favorite crusines may play more of a role in our health than what you may think. "Interest in the potential neuroprotective properties of curcumin rose after studies found very low levels of neurological diseases, such as Alzheimer's disease, in elderly Indian populations. Added to this were studies confirming curcumin as a potent anti-inflammatory agent, effective in wound healing. And just last fall, researchers at the University of California, Los Angeles reported that curcumin appeared to slow the progression of Alzheimer's disease in mice. In their 30-day study, Dr. Natarajan and co-researcher Dr. John Bright administered 50- and 100-microgram doses of curcumin, three times per week, to a group of mice bred to develop experimental autoimmune encephalomyelitis (EAE). They then monitored the mice for signs of MS-like neurological impairment. In contrast, mice given the 50-microgram dose of the curry compound showed only minor symptoms, such as a temporarily stiff tail. And mice given the 100-microgram dose appeared completely unimpaired throughout the 30 days of the study. The results did not surprise Dr. Natarajan. In Asian countries, such as India and China, where people eat more spicy foods and more yellow compounds like curcumin, reports of MS are "very, very rare," he pointed out. He said the doses the mice received were roughly equivalent in human terms to those found in a typical Indian diet." How can I fight PMS naturally? "I always emphasize self-care in every health context, and nowhere is it more important than with PMS. Make sure that you're getting plenty of aerobic exercise -- it really helps. Reduce salt if you're bloating and caffeine if you're frenzied or irritable. And a reduction in simple carbohydrates like sugar and starches helps, as does "grazing" with several small meals instead of three big ones. If you have chocolate cravings (who doesn't?), succumb sensibly with tiny bits of quality, preferably dark chocolate to maximize flavor and "feel-good" chemicals while reducing the fat and sugar liability. I advise Vitamin B-6 since it helps with carbohydrate metabolism, the formation of neurotransmitters and assists with the stress response. But limit intake to 100 mg. daily over long periods. An occasional boost to 150-200 mg. before periods for a few days won't hurt, though, and may help. Calcium and magnesium are both worth a try; shoot for 1200 mg and 400 mg respectively. For breast tenderness, try Evening Primrose Oil, but expect results slowly. Essential fatty acids like EPO are underrated nutritional supplements. Progesterone creams and over-the-counter remedies are widely touted, and while I don't have a problem with trying reliable products, you may end up spending a lot for a placebo effect. But one botanical has the Dr. T "Seal of Approval". Last year the British Medical Journal published a study on Chaste berry fruit extract (Vitex agnus castus), validating it as a legitimate PMS option. It alters hormonal flux and is said by herbalists to "balance" female hormones. Irritability, mood change, anger, headache and breast tenderness improved more than 50% in half the women. This is a time-honored treatment and I recommend it frequently. Be careful about quality and always check with your doctor before self-medicating to avoid interactions and untoward side effects." What type of headache do you have? Take the quizz to find out. American Council for Headache Education Have a headache or a migraine? I added this just in case you have a headache (like I had all day) and want to research information about headaches. National Headache Foundation More information on all types of headaches plus support groups (in case the headache is that bad or if you just want to ask a question). Society of Neuroscience Brain Briefings-lots of good links & articals related to the brain. Brain quiz "Your brain is amazing — Did you know that? An incredibly complex system, it is the control room of your body. This quiz tests your IQ when it comes to knowing about that all-important "gray matter."" BrainSource "includes a broad and growing collection of information and resources about normal and injured brains, clinical and forensic neuropsychology, brain injury rehabilitation, creativity, memory and other brain processes, education, brain-body health, and other topics in brain science. BrainSource is also a guide to products, books, continuing education, and Internet resources in neuroscience." BrainPlace.com Daniel G. Amen, MD web site. He has "been involved in brain imaging research for the past 13 years, pretty much on a daily basis. First with sophisticated quantitative EEG (brainwave) studies, and in the last 10 years with a nuclear medicine brain study called SPECT (single photon emission computed tomography) which measures cerebral blood flow and metabolic activity patterns." This site has a wealth of information on the brain and conditions that effect the brain. He even has a test he developed Amen Brain System Checklist. Take it & see how you score on cognitive querks. American Association of Christain Counselors "AACC exists to help professional, pastoral and lay caregivers provide effective Christ-centered soulcare for those seeking direction in life." Advanced Brain.com "Advanced Brain Technologies is the creator of innovative brain-based products and technologies for therapeutic, educational and self-improvement benefits." Brain.com Site contains information & news on various brain diseases as well as interesting information related to the brain and various products to promote a healthier brain. As with any products the sales pitch often promises more than what the product delivers. If you are tempted to buy something, first check it out, sleep on it & pray about it. The Four Brain States Site sent to me by my sister. "Beta Alertness Concentration Cognition You are wide-awake, alert. Your mind is sharp, focused. It makes connections quickly, easily and you're primed to do work that requires your full attention. In the Beta state, neurons fire abundantly, in rapid succession, helping you achieve peak performance. New ideas and solutions to problems flash like lightning into your mind. Beta training is one of the frequencies that biofeedback therapists use to treat Attention Deficit Disorder. Beta waves range between 13-40 HZ. The Beta state is associated with peak concentration, heightened alertness, hand eye coordination and visual acuity. Alpha Relaxation Visualization Creativity When you are truly relaxed, your brain activity slows from the rapid patterns of Beta into the more gentle waves of Alpha. Your awareness expands. Fresh creative energy begins to flow. Fears vanish. You experience a liberating sense of peace and well-being. In biofeedback, Alpha training is most commonly recommended for the treatment of stress. Alpha waves range between 7-12 HZ. Theta Meditation Intuition Memory Going deeper into relaxation, you enter the elusive and mysterious Theta state where brain activity slows almost to the point of sleep, but not quite. Theta is the brain state where magic happens in the crucible of your own neurological activity. Theta brings forward heightened receptivity, flashes of dreamlike imagery, inspiration, and your long-forgotten memories. Theta can bring you deep states of meditation. A sensation of "floating." And, because it is an expansive state, in Theta, you may feel your mind expand beyond the boundaries of your body. Theta waves range between 4-7 HZ. Delta Detached Awareness Healing Sleep Long, slow, undulating. Delta is the slowest of all four brain wave frequencies. Most commonly associated with deep sleep, certain frequencies in the Delta range also trigger the release of Human Growth Hormone so beneficial for healing and regeneration. This is why sleep - deep restorative sleep - the kind that Delta frequencies help induce is so essential to the healing process. Delta waves range between 0-4 HZ." Neurosciences on the Internet Epilepsy and Seizures links to many sites. Epilepsy Foundation "Epilepsy:sometimes called a seizure disorder, is a chronic medical condition produced by temporary changes in the electrical function of the brain, causing seizures which affect awareness, movement, or sensation. The Epilepsy Foundation will ensure that people with seizures are able to participate in all life experiences; and will prevent, control and cure epilepsy through research, education, advocacy and services." American Stroke Association You can search their journal for any topics of interest pertaining to strokes. 

|